
My heart sunk. Paralysed. Frozen in time and space yet transported to a time before. And then the tears.
Hearing the news of Chris Hoy’s terminal diagnosis of prostate cancer at the age of 48 threw me back to the turmoil I had experienced in 2003 – my annus horribilis. It instigated a burning need to tell (re-tell) the story of early onset prostate cancer which changed my life – and the life of the people I most care about.
This is a not simply another lived experience story about prostate cancer, but a reminder of the importance of a critical understanding of knowledge and evidence, so called “expertise” and how health/medical protocols and guidelines are developed.
Twenty one years ago, the year I turned 40 years of age, my father in law (aged 66) was diagnosed with prostate cancer. His brother had, a few years earlier, died of prostate cancer. Like Chris Hoy, he had visited his GP for a persistent pain, in his case in his leg. He was diagnosed with terminal Stage 4 prostate cancer and died, if my recollection is correct, within a few months
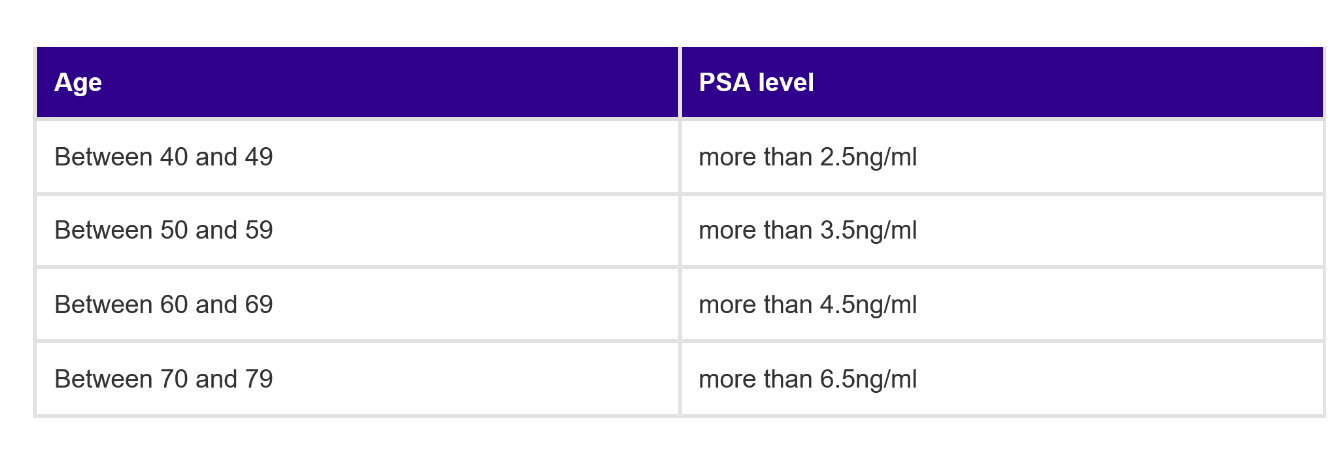
While my father-in-law underwent radiotherapy, my partner was called for his routine annual health check-up. Given his father’s recent diagnosis, he was offered a PSA test. He was 40 years of age. Although ambivalent – he had no symptoms and it seemed somewhat pointless to him – he took up the offer. The result returned an abnormal reading of around 7ng/ml.
The follow-up, much resisted, DRE (digital rectal examination) found nothing abnormal - a lovely, small, smooth prostate! I delved into the literature about prostates and PSA tests. A biopsy was arranged. Six samples were taken; no signs of cancer were found. My partner’s relief was palpable, and he resumed life as normal, noting the suggested repeat PSA test in six months’ time.
Not me though. Far, far too many unanswered questions for me. Totally dissatisfied with the state of play.
Prostate Specific Antigen is a protein produced by both normal and cancerous prostate cells. All men have some PSA in their blood. The PSA test is a non-specific test. It does not detect cancer. It detects the levels of PSA in the blood. Abnormal or heightened functioning of the prostate gland increases the amount of PSA produced. As men get older, their prostate gets larger, more PSA is produced. If there is inflammation, infection or disease (benign or otherwise) – there is more PSA in the blood stream.
My partner did not have inflammation. He did not have any prostate disease. He was 40 years old. Why was his PSA elevated? No-one could give me the answer. I devoured the academic papers from all over the world – even those not written in the English language. None gave me a satisfactory answer. A shrug of the shoulders from those who “should” know was not good enough. I cared deeply for the father of my three children, and I was scared.
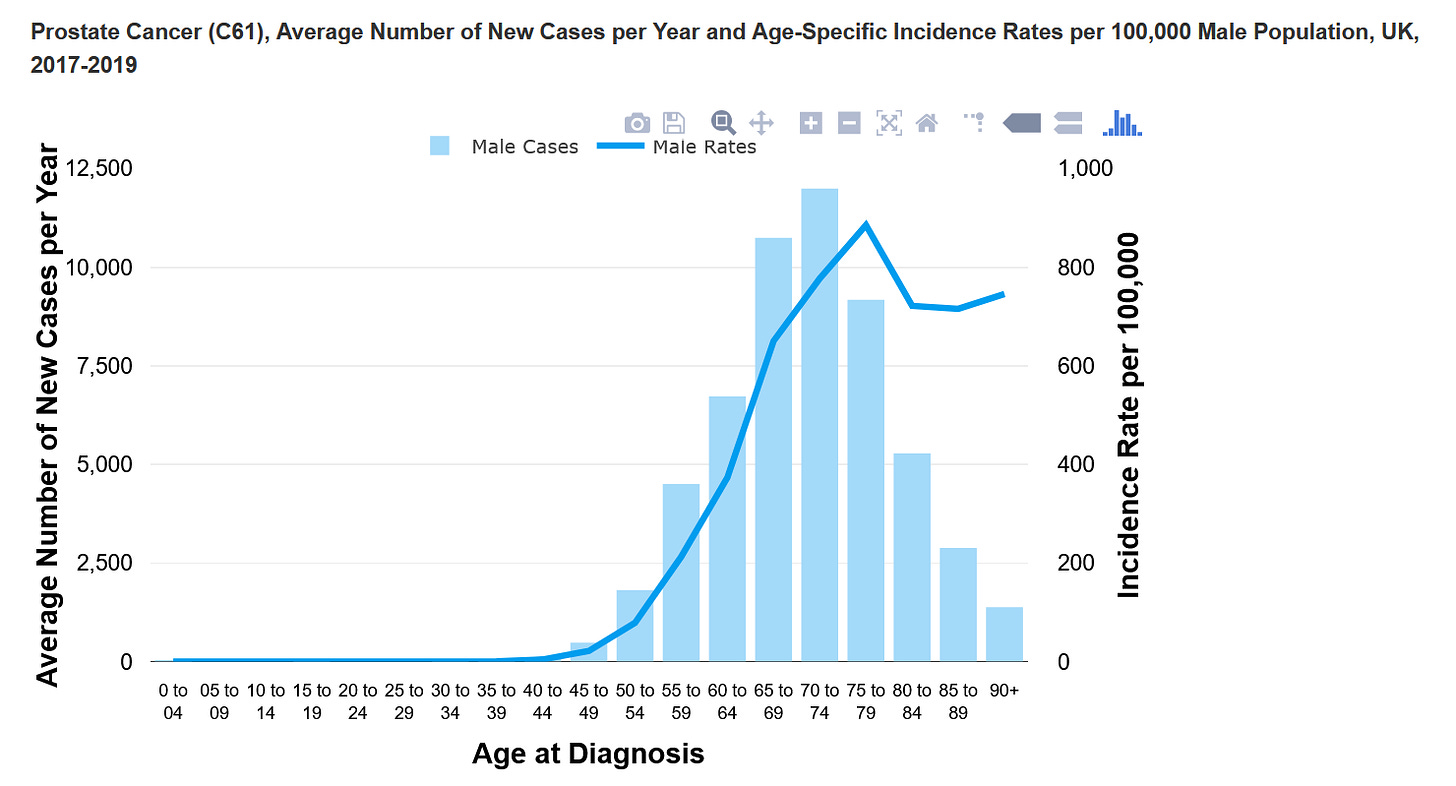
I hit the protocols which dictated how prostate disease was managed and read every piece of evidence which shaped the recommendations. The protocols were based on the prevalence and incidence of prostate disease and prostate cancer specifically, being a condition of older men – 65, 70 older. The protocols were based on sound evidence that, for the vast majority of men, prostate cancer has a late in life onset, is often a mild, slow progressing cancer, which the majority of men die with, rather than of.
But my partner was 40. There was a strong familial history – his father and his uncle – what did the protocols say of this? Very little.
While the protocols have been updated since then, there is still little reference to any research of younger men with prostate cancer. Young men are subsumed in a category of under 60, or under 65.
When the follow up PSA test six months later returned a still elevated PSA level, the advice was sit back and have another test in 6 months. My partner was happy with this. He was fit and well, nothing to worry about.
Me? I was consumed with angst and frustration. Fearful. Convinced my partner had prostate cancer and no-one seemed to care. Worried about how I would raise our three children on my own because he was surely going to die. Catastrophising? Oh yes!! Definitely! But …. Why did my partner have a PSA of 7? Tell me that please. Give me more than a shrug of your shoulders ….
There is that quote, isn’t there, attributed to Conan Doyle’s Sherlock Holmes. “When you have eliminated all which is impossible, then whatever remains, however improbable, must be the truth.”
No prostate disease; no inflammation; lovely smooth prostate – so what the fuck is producing the elevated PSA???
I knew by now how rare prostate cancer was in a man of 40 years of age. At that time around 3 cases a year were diagnosed in men aged 40-44 in the UK; currently there are around 90 cases a year. I knew my partner had an elevated risk given his family history. I could not just sit tight while the “experts” followed NICE guidelines or existing protocols which had not been developed with my partner in mind. Guidelines developed without the inclusion of research on rarer cases of prostate cancer in younger men.
My partner did not want to hear my concerns. He was fine!! If he had cancer there would be physical signs, pain - something? Nothing wrong with his urine stream!
So I made an appointment with my partners’ consultant to speak with him about my concerns – alone. He listened, acknowledged my concerns, and said the only option available would be a very painful saturation biopsy – where the prostate was sampled more widely. He didn’t recommend this, but acknowledged that my concern around the elevated PSA level was valid. While the saturation biopsy was an option, he felt it was appropriate to wait another six months and review the PSA level again.
There followed months of me badgering, cajoling, begging my partner to consider the saturation biopsy … met with a huge lack of enthusiasm and resistance from him. I felt shitty about my behaviour, but could not dispel a now firmly held belief - based on my comprehensive, critical analysis of the literature - that the only explanation for the elevated PSA level was an undiagnosed tumour. As for him? He was fit and well, the “experts” didn’t seem concerned; why on earth would he want to put himself through this ordeal?
I wore my partner down. He agreed, reluctantly, to the saturation biopsy. Out of the twenty cores taken – just one indicated the presence of cancer. After considering treatment options, a radical prostatectomy was arranged.
On removal of his lovely, small, smooth prostate – bilateral, Gleason 7 cancer was found filling two thirds of the prostate. Crucially – it had not escaped the prostate and was contained.
As the coverage of Chris Hoy fills my TV screen, social media and news feeds, I am revisited by the thought that if I had not been so inquisitive and persistent – my children may not have had their father here now, 21 years later.
There is currently no screening programme for prostate cancer in the UK – largely due to the non-specificity of the PSA test and risks of false positives and false negatives. 1 in 50 men with a normal PSA level have a fast growing prostate cancer.
Currently men over the age of 50 can request a PSA test from their GP. But this would not have helped Chris Hoy – nor the father of my children.
There are currently around 580 men a year diagnosed with prostate cancer under the age of 50 in the UK and around 18 deaths in this age group.
The PSA test IS imperfect, but knowledge is key and perhaps this imperfect test remains the best weapon for young men with a familial history of prostate cancer until more effective testing and screening is developed. The risk of cancer is 2-4 times higher in men who have a close relative with the disease, and is higher in men aged under 65. And it is not just familial male cancers which increase risk. Prostate cancer risk is 19-24% higher in men whose mother had breast cancer, and the risk is up to 5 times higher in men with BRCA2 mutation – 7 times higher for those aged under 65. More aggressive cancers have been linked to gene mutations, including the BRCA2 gene. Black men also have a greater risk of prostate cancer in general, as well as disease at a younger age.
Following the courage of Chris Hoy in sharing his story, there are renewed calls for PSA tests to be available from the age of 45, and for more pro-active conversations from medical professionals. Yet this would still not have helped Chris, or my partner, who but for the coincidental timing of his father’s diagnosis and his routine private health check-up may not have had his PSA tested.
While this is not a recommendation, knowing that he has an elevated risk, that his dad was diagnosed at 40 – my son has been having his PSA measured annually, since the age of 25. He knows his normal – his baseline. Any deviation from this will be an early warning sign – an alert to check things out.
1 in 8 men will have prostate cancer in their lifetime. For many, like my recently diagnosed dad (aged 81), it is a not unexpected consequence of aging – like several other cancers. While diagnosis can naturally bring anxiety, treatment – if needed – is often manageable and well tolerated.
For those with higher risk of early onset cancer, we must do better. Diagnostic imaging and biopsy have come some distance in the last 20 years. Promising new breakthroughs are on the horizon, thanks to some fantastic research. We must provide the best opportunity of early detection and diagnosis to ensure the earliest treatment and best possible outcomes. We must insist on guidelines and protocols which include research on familial and early age prostate cancer. We should expect no less for our men, than the advances which we have seen for the women in our lives with breast cancer screening and treatment.
You can check your risk of prostate cancer NOW – simply and quickly with Prostate Cancer UK’s risk tool here.
You can also support Prostate Cancer UK’s call for the revision of the outdated NHS guidelines here.




Great and important blog, Sue. Getting doctors and the public to raise awareness like you did in the face of general ignorance. Doing more screening for (at least the at risk) younger men. Then personally hunting down the evidence and your own male loved-ones. And more generally men need to wise up logically and emotionally to value their health and lives more … led, as it seems necessary, by how women do it! 😏😑 …
Which seems to link to an old story of more aggressive male resistance to the challenge of bright bold sensible women: the Edinburgh 1870 riot. Link below.
That riot is echoed by modern day sex and gender protests - in Edinburgh too. Kind protection of the vulnerable is given as the motive, but the women didn’t accept the category of victim. So they suffered the consequences of disobedience.
Isn’t Chris Hoy also far too laid back in how he’s accepting the consequences of cultural and medical ignorance?
https://blogs.ed.ac.uk/edmedtimeline/the-surgeons-hall-riot-a-turning-point/